SMISS 2020 Presentation
Return to Work Status after Cervical Disc Replacement — Worker’s Compensation Population
Followed 13 work comp patients — mixture of 1 and 2 level replacement surgeries
Average time to return to work with restrictions was 60 days and 69.9 days without restrictions
Cervical disc replacement has the potential to improve the quality of life for patients suffering from neck and arm pain. It offers unique benefits compared to cervical fusion surgery, including a more rapid recovery rate and a faster return to work
To our knowledge this is the only study to review return to work status after cervical disc replacement in the worker’s compensation population.
Return to Work Status after SI Joint Fusion — Worker’s Compensation Population
15 work comp patients
Average time to return to work with restrictions was 55 days
5 patients returned to work full duty an average of 94 days after surgery
SI Fusion has the potential to improve the quality of life for patients suffering from low back pain.
To our knowledge this is the only study to review the return to work time after SI Joint Fusion in the worker’s compensation population.
Safety of the Addition of a Perioperative Electrolyte Drink to Enhance Recovery After Spine Surgery - Protocol
Gave 32 oz of electrolyte drink at midnight before surgery day; and, 8 oz electrolyte drink the day of surgery
No aspirations were observed
We have demonstrated the safety of utilizing this cost-effective addition to the perioperative anesthesia protocol.
Further study will need to be performed in a larger prospective multicenter trial for both hospital based and outpatient spine surgery to further validate patient satisfaction and the safety profile of this strategy.
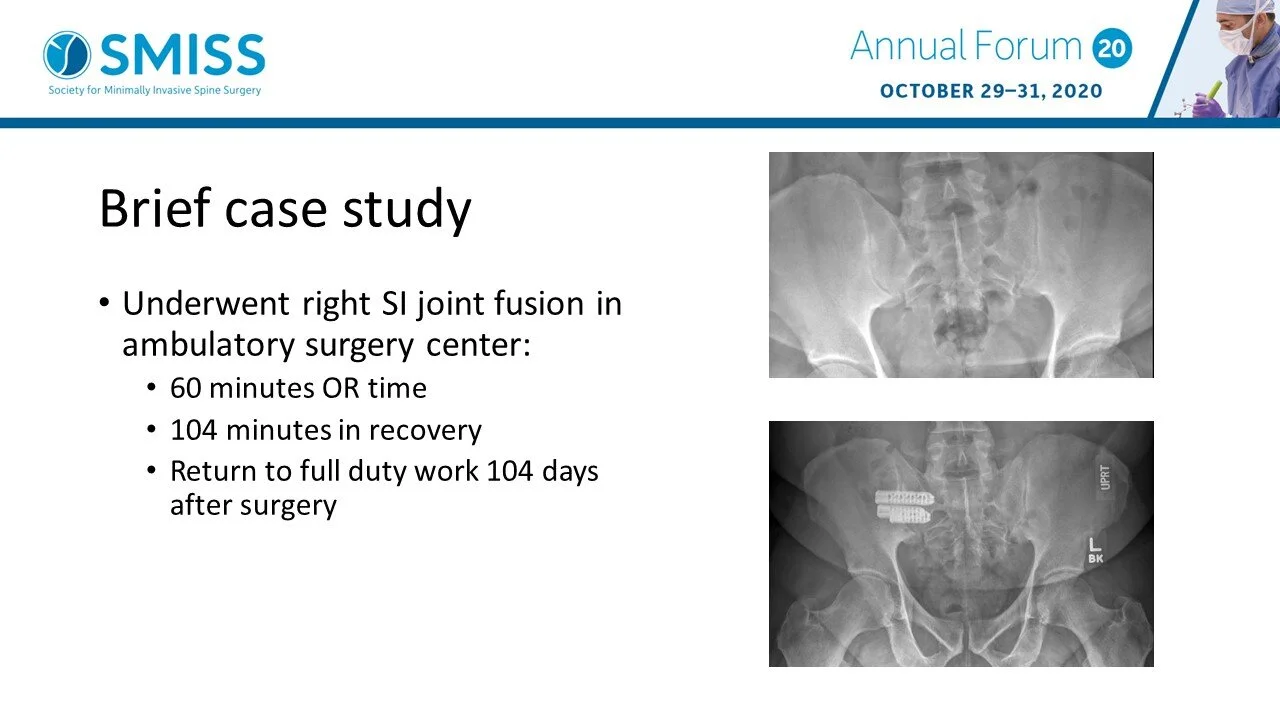
Safety and Reproducibility of Sacroiliac Joint Fusion in an Ambulatory Surgery Center
Followed 19 patients - mixture of private insurance and work comp/liability
Average length of stay was 102.5 minutes after surgery.
No blood transfusions. No hospital readmits within 30 days. No infections noted.
The potential to move SIJF to the outpatient setting, utilizing advanced minimally invasive surgery, presents a significant opportunity for patients and payers to benefit from decreased infection rates, quicker recovery and achieve cost benefits.
To our knowledge this is the first data on outpatient minimally invasive SIJF. Our early data suggests that in well selected patients, the SIJF procedure can be performed safely and be reproduced in the outpatient setting.
Further research performed in a prospective multi-center study is needed to validate the early findings.
Unilateral Expandable Interbody Cage Placement — Minimally Invasive Midline Fusion
A retrospective chart review was performed on 16 consecutive patients who underwent a midline lumbar fusion utilizing a single expandable interbody device.
Post-operative radiographs were examined to determine device position, relative to the vertebral bodies.
Device positioning was graded A, B, or C based on the presence of device midline in the medial, middle or lateral third of the superior vertebral body
9 devices were graded "A"; 8 devices were graded "B". None received a grade of "C"
Many surgeons have preferred to utilize a single cage for minimally invasive fusions. The use of a single cage presents a significant challenge as it is difficult to obtain a 30-45 degree angle in order to position the cage in the middle third of the vertebral body
The advantage of the expandable lordotic oblique cage for this procedure is the placement of the cage in the optimal radiographic position prior to expansion
Further research examining subsidence and fusion rates as well as segmental lordosis utilizing this modified midline fusion procedure requires exploration.
Accuracy and Reoperation Rate - cortical bone trajectory screws utilizing the cannulator technique
Review of 1503 screws placed utilizing the cannulator technique since 2014
5 screws required repositioning, with an overall replacement rate of 0.4%, or a 99.6% accuracy rate
There have been many previous studies looking at the placement of freehand standard trajectory pedicle screws, compared with robotic navigated placement.
This is the first paper that has looked at revision rates for malpositioned cortical screws.
PUBLISHED PAPERS
Add list here